Endoscopic Spine Systems
Spine Endoscopy Equipment from elliquence
Endoscopic Spine Surgery is gaining in popularity among clinicians looking to improve outcomes and patient satisfaction.
elliquence®, LLC, is the leading expert of Radio Wave Solutions with the Surgi-Max® Ultra RF Generator and the original Trigger-Flex® directional RF handpiece. Together now with simple, smart, and comprehensive Endoscopic Spine Systems, elliquence offers clinicians the full ability to perform endoscopic procedures with approaches for Transforaminal, Interlaminar, Rhizotomy, and Spinal Stenosis.
Endoscopy Technology for Spine Conditions & Surgery
Our endoscopic spine technology allows medical professionals to safely and efficiently perform endoscopic procedures to treat spine conditions. Whether you are a spine surgeon at a hospital or a doctor in your own practice, our endoscopy equipment can help you treat a range of spinal conditions and injuries, such as disc herniations.

Transforaminal Endoscopy
Endoscopic Facet Denervation
Endoscopic Spine Surgery: A Surgeon’s Advantage with Minimally Invasive Spine Care
Introduction
As a spine surgeon committed to delivering outstanding patient outcomes, staying at the cutting edge of technology and technique is essential. Endoscopic Spine Surgery (ESS) represents a paradigm-shift in spinal treatment, offering you the opportunity to enhance your surgical performance, reduce patient morbidity, and position your practice at the forefront of minimally invasive spine care.
In this page you’ll discover the surgeon-centric benefits of ESS: improved precision, faster procedural flow, better patient recovery metrics, practice-differentiation, and long-term strategic advantages.
Why Surgeons Are Embracing Endoscopic Spine Techniques
-
Less collateral tissue damage: ESS uses a tiny working channel/endoscope through minimal incisions, so muscle and ligament disruption is dramatically reduced compared with open surgery. mayoclinic.org+2PMC+2
-
Improved intraoperative visualization & precision: With high-definition endoscopic optics, you gain enhanced views of target anatomy (nerve roots, foramina, disc fragments) which supports more accurate decompression or disc removal. sciatica.com+1
-
Lower intraoperative morbidity: Studies show ESS is associated with significantly less blood loss, reduced hospital stay, and fewer complications in many cases when compared to open approaches. PMC
-
Faster patient recovery translates to practice productivity: Because patients recover quicker, require fewer inpatient days or narcotics, and can return to activity sooner, you are able to improve throughput, referral satisfaction and operational efficiency. Minnesota Spine Institute+1
-
Opportunity for outpatient/ambulatory models: Many ESS cases can be performed on an outpatient basis or with minimal hospital stay, aligning with value-based care models and payer/regulatory pressures. USF Health+1
-
Strategic differentiation & future-proofing your practice: As the spine surgery market evolves toward less invasive, tissue-sparing techniques, adopting ESS positions you as a leader, improves referral pathways (surgeons, physiatrists, spine centres) and supports growth in an environment of rising cost and patient expectation. mayoclinic.org
Key Benefit Areas for Surgeons
1. Enhanced Surgical Workflow & Or Efficiency
-
Smaller incisions and minimal retraction reduce setup and closure time, sometimes allowing same-day discharge. UW Medicine
-
Because less tissue manipulation is required, intra-operative fatigue and surgeon stress may decrease, improving performance consistency.
-
Reduced need for hardware (in some cases) or extensive fusion may simplify instrumentation logistics and cost implications. Brown Health
2. Improved Patient Outcomes & Satisfaction
-
Less post-operative pain and faster mobilization mean happier patients, better recovery metrics and stronger referral network. Minnesota Spine Institute+1
-
Reduced risk of infection, fewer complications and less hospital-related morbidity strengthen your risk profile and outcome track-record. OSF HealthCare
-
Better cosmetic results (smaller scars) and quicker return to work/life drive patient satisfaction and positive reviews. khuranaspine.com
3. Broader Case Mix & Access to Higher-risk Patients
-
ESS’s minimally invasive nature may allow you to treat patients who are higher risk for open surgery (older age, comorbidities) and expand your referral base. mayoclinic.org
-
Endoscopic techniques are also valuable in revision settings (avoiding scar tissue) where open approaches carry increased morbidity. PMC
4. Cost-Effectiveness & Value-based Care Alignment
-
Shorter hospital stays, less time under general anesthesia, fewer post-op resources and quicker return to function can reduce overall cost per case — aligning with payor and hospital value-based models. PMC
-
Presenting ESS as an offering in your practice can help you engage hospitals and ambulatory surgical centres looking for shorter-stay, high-throughput spine cases.
5. Practice Growth, Branding & Competitive Advantage
-
By offering ESS, you send a message to referring physicians, patients and payors that you are skilled in true minimally invasive spine techniques — enhancing your referral pipeline.
-
With rising patient awareness and demand for “least invasive” options, you create a differentiator in a crowded market.
-
In the era of social media and digital marketing, ESS allows you to highlight fast recovery, minimal scarring, same-day discharge — compelling content for surgeons, staff and patients alike.
Implementation Considerations for the Surgeon
-
Training and proficiency: Transitioning to ESS requires dedicated training, a learning curve and equipment hardware investment. Published literature notes the learning curve may be lower for biportal vs uniportal techniques, but commitment to case volume and safety protocols is key. PMC+1
-
Case-selection protocols: Not all spinal pathologies are suitable for endoscopic techniques (e.g., severe instability, complex deformity, large multi-level disease). Proper patient selection is critical for outcomes and adoption. farnorthsurgery.com+1
-
Equipment and instrumentation: Endoscopic systems, dedicated portals, camera systems, irrigation control and specialized instruments are required. Partnering with your device/technology provider (such as elliquence) to ensure setup is integrated is fundamental.
-
Workflow alignment: To maximize benefits, align OR scheduling, same-day discharge protocols, pre-op and post-op pathways (pain management, mobilization) to reflect the reduced trauma profile of ESS.
-
Outcome tracking and marketing: Monitor surgical metrics (blood loss, length of stay, narcotic usage, return to work) and use these data in peer outreach, marketing and referring-physician education to underline your excellence in ESS.
Why Elliquence Is Your Partner for Endoscopic Spine Excellence
At Elliquence, we recognise that delivering true minimally invasive spine solutions requires more than a tool — it requires a platform, training, and support. With our endoscopic-first mindset and suite of devices designed for precision, tissue preservation and surgeon ergonomics, you gain access to:
-
A comprehensive training curriculum and fellowship-level education in endoscopic spine techniques.
-
Integrated instrumentation, operative workflows and support services tuned for endoscopic spine surgery.
-
Marketing and patient-education collateral that helps you position your practice as the “Least Invasive Procedural Solutions” leader.
Together, we help you bridge the gap from uniportal to biportal endoscopic spine techniques, elevate your procedural repertoire and drive growth in the evolving spine surgery domain.
Common FAQs for Surgeons Considering Endoscopic Spine Surgery
Q: Is the success rate the same as open surgery?
A: Emerging evidence suggests that for appropriately selected cases, ESS achieves comparable success rates to open or microscopic decompression, with the added benefit of lower tissue trauma and complications. PMC
Q: Does ESS require more time in the OR?
A: Initially, there may be a modest increase in time due to the learning curve; however, many centres report equal or shorter OR times once proficiency is established, and hospital-stay time is typically reduced. Houston Methodist
Q: What about fusion cases?
A: While much of the current ESS literature centres on decompression and disc herniation, endoscopic interbody fusion techniques are being developed and show promise in selected cases. PMC+1
Q: Are there limitations?
A: Yes — multi-level complex deformity, high BMI, severe instability or infection may still require open or conventional minimally invasive approaches. Accurate case-selection remains essential. New Jersey Spine Specialist
Take the Next Step
If you’re ready to elevate your spine surgery practice, reduce patient recovery times, and position yourself as a leader in minimally invasive spine care, contact us at elliquence. Let’s explore how endoscopic spine surgery can transform your surgical practice and deliver measurable difference to patients and your institution.
elliquence Endoscopic Instrumentation
Endoscopes
Avialable for all approaches

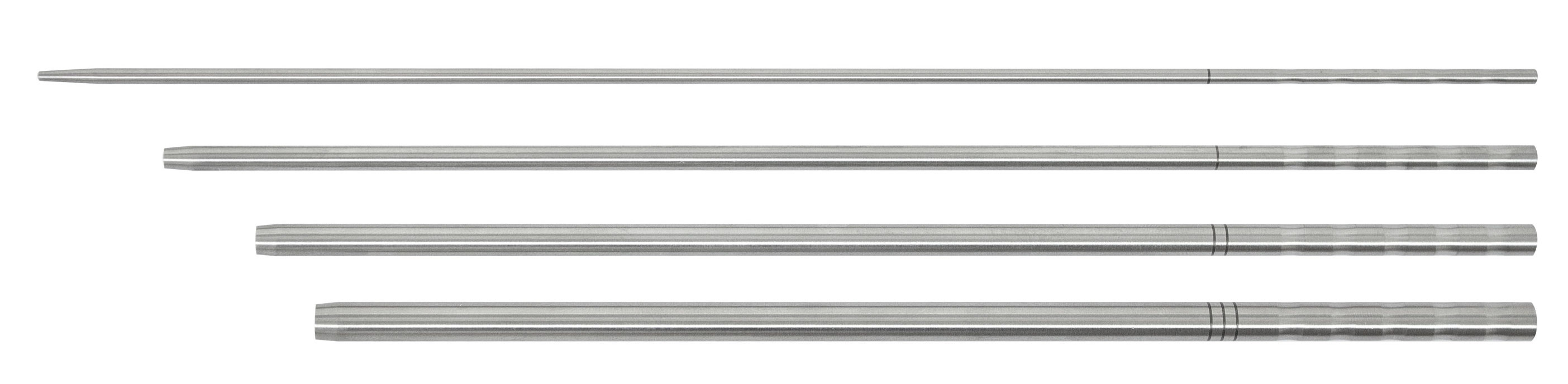
Dilators / Coaxial Step Dilators
Available in a variety of sizes

Graspers
Available in a variety of types and sizes


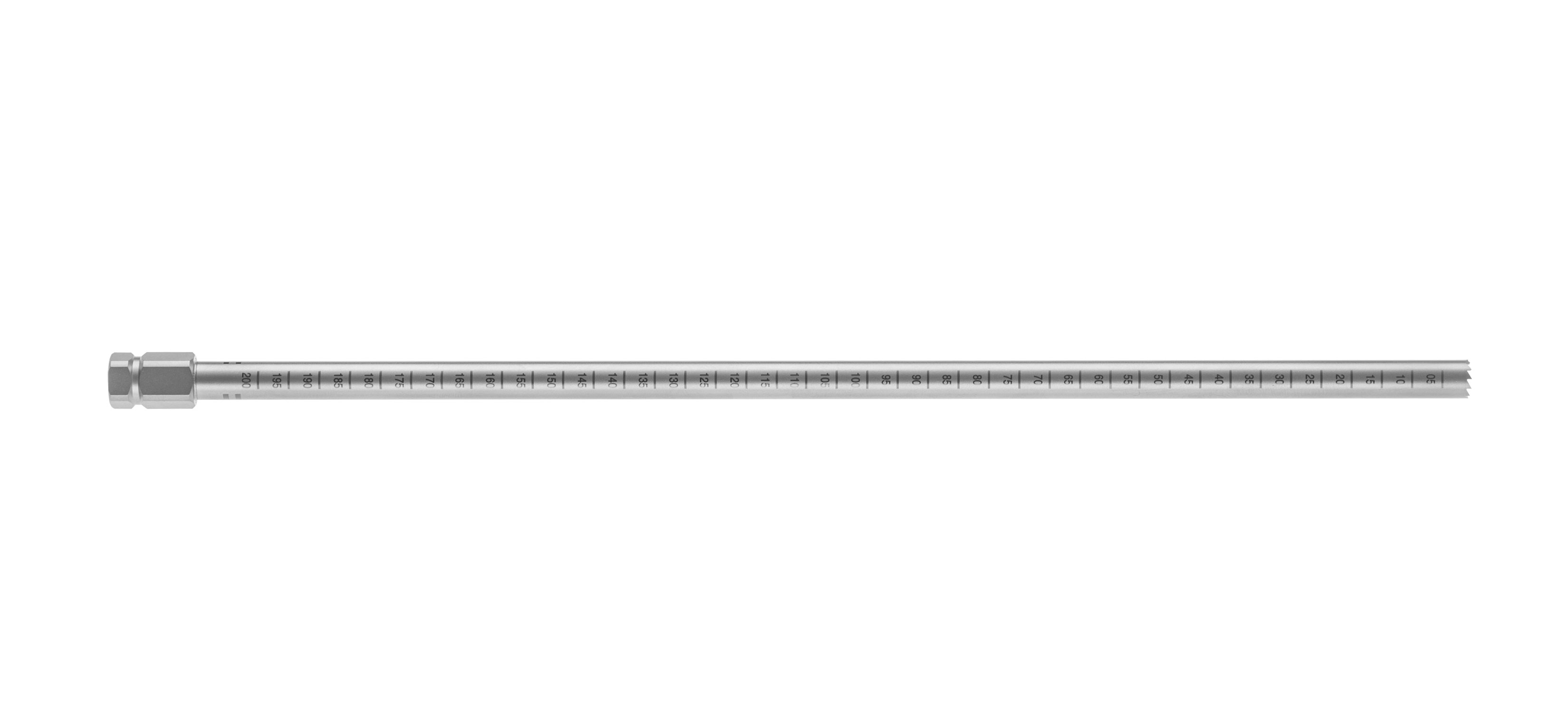
Working Tubes
Available in various sizes and types



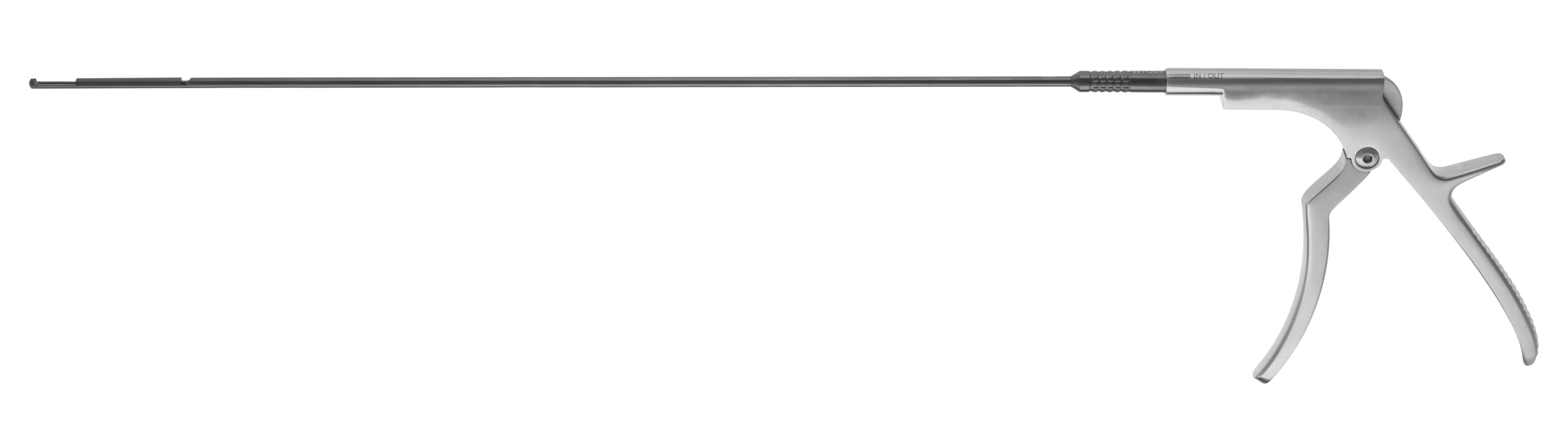
Kerrisons


Trephines

Incorporate elliquence Medical Technology Today
Endoscopic spine surgery is a minimally invasive procedure that surgeons perform to treat a range of spine conditions. Our Endoscopic Spine Systems help medical professionals treat patients quickly and efficiently with minimal scarring and recovery time. Contact elliquence online or call us at 516-277-9000 today to discuss to learn more about how you can implement our Endoscopic Spine Systems.
Gun Choi, MD
elliquence technology
“An important consideration for anyone doing endoscopic surgery is how to ablate tissue and create hemostasis. Not all methods are created equal and I have found over the last 15 plus years that elliquence’s technology is trustworthy and performs better than other RF machines, allowing me to achieve better results. elliquence technology cleanly and efficiently ablates the tissue while controlling hemostasis very effectively, and as a result is a key component in excellent patient outcomes.”

Nicholas Prada, MD
Approach on Interlaminar
The interlaminar window at L5-S1 is easily accessed through a direct posterior approach, visualized using both AP and Lateral radiographs. The lateral facet is located and the stab incision is made directly medial to the facet to the level of the fascial layer. The dilator is introduced to the level of the ligamentum flavum, confirming AP and Lateral radiographs. The cannula is introduced over the dilator with the bevel open medially and the endoscope is introduced. Various instruments including the Trigger-Flex® RF probe are used to expose the ligamentum flavum. Punches and kerrisons can now be used to perforate the ligamentum for access to the spinal canal. The nerves are visualized and mobilized using a dissector. The canula is rotated to further mobilize, retract and protect the nerves exposing the herniation. A variety of instruments along with the Trigger-Flex® RF probe can now be utilized to remove disc material. The small wound site can be closed with minimal suture or steri-strips.

Jim Yue, MD
Approach on Transforaminal
Patient selection is critical to the success of any surgical approach, the herniated disc tissue must be accessible through the foramen. Patient is positioned in the prone position on either bolsters or a Wilson frame to open up the foraminal space. AP and Lateral radiographs are used to identify the targeted foraminal levels. If an intra-discal approach is elected, an 18 gauge spinal needle is initially introduced not past the medial edge of the pedicle AP view, and in the posterior 3rd of the disc space in the lateral view with care being taken to avoid the exiting nerve root. The guide wire is transferred through the needle and a stab incision is performed along the guide wire. The dilator is introduced over the guide wire to the level of the annulus, again care should be taken to avoid the exiting nerve. The beveled cannula is introduced over the dilator creating a working portal for the introduction of the endoscope for direct visualization, light, irrigation and working access to the previously identified pathology. Upon completion of the surgery, the small wound can be closed with either steri-strips or a single stitch.

Jorge Ramirez, MD
Approach on Rhizotomy
Endoscopic Dorsal Ramus Rhizotomy is a procedure that can provide patients with relief of pain associated with degenerative disease of the facet joints. Use of the spine endoscope provides visualization of the posterior spinal anatomy and nerves, while an endoscopic RF probe facilitates the ablation of the medial (and lateral) branches of the dorsal ramus and can lead to more complete ablation of the nerves and therefore better and longer lasting pain relief. Endoscopic Rhizotomy is most effective in those patients who have experienced greater than 50% relief of pain with medial branch blocks. The Endoscopic Dorsal Ramus Rhizotomy procedure offers an alternative for addressing axial back pain that is much less invasive than spinal fusion. A Rhizotomy is primarily done at the junction where the medial branch of the dorsal ramus nerve crosses over the transverse process of the vertebral body, however to make sure a complete ablation is accomplished rotating the RF probe through a full 360˚ ensures a complete evulsion of the nerves is achieved.

Stefan Hellinger, MD
Approach on Stenosis
Lumbar spinal stenosis is a common cause of radicular and generalized back pain among older adults. Endoscopic minimally invasive surgery, in contrast to open decompression, may provide the opportunity for a less invasive surgical intervention. Visualization and illumination during the operation can be optimized. Since a more extensive bone or ligament resection is frequently necessary here, a larger diameter endoscope with a correspondingly larger endoscopic working channel and larger instruments and burrs are necessary. After the access has been created, the bony structures are exposed. It may be helpful to start decompression at the caudal end of the descending facet. Depending on the pathology, decompression is then commenced with resection of parts of the medial descending facet, the cranial and caudal lamina, and the ligamentum flavum. The extent of decompression generally continues cranially at least until the tip of the ascending facet and caudally to half of the pedicle. The medial portions of the ascending facet and the ligamentum flavum are then resected until sufficient decompression of the neural structures can be clearly seen. In the case of a central stenosis, the ligamentum flavum generally needs to be resected medially to the midline. If the patient experiences bilateral symptoms of stenosis, an “over the top” access using the undercutting technique to the opposite side is carried out.
